The Women’s Health Gap Has Been Significant
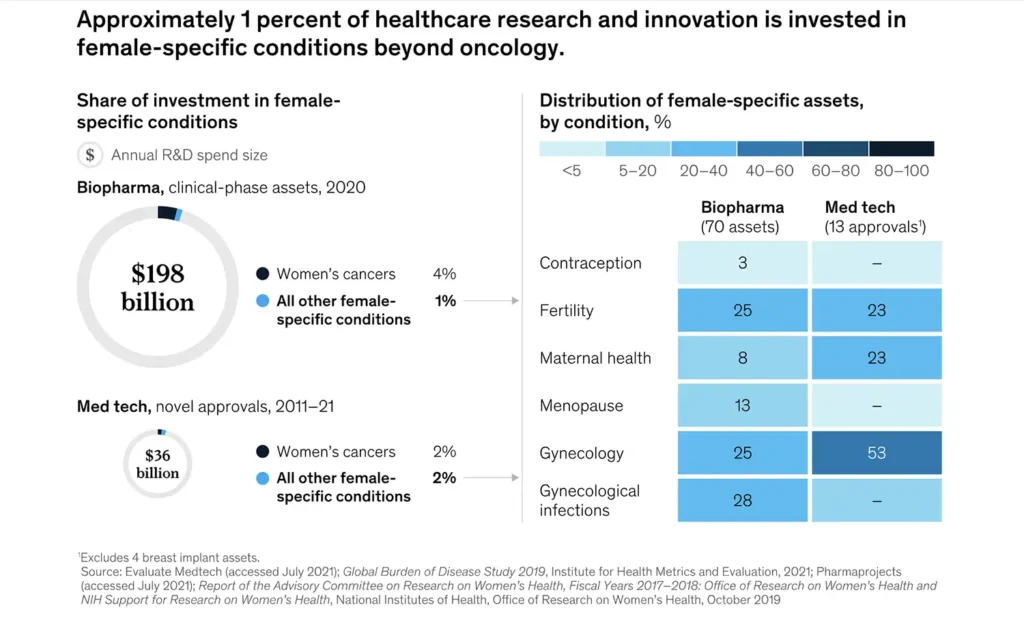
The women’s health gap has remained persistent over the years, with women being underdiagnosed for certain conditions compared to men. We have a significant historical data gap when it comes to female bodies versus male bodies, as medical research has assumed that male bodies can represent humanity as a whole. In 2020, only one percent of healthcare research, development and innovation was invested in female-specific conditions, aside from oncology, according to McKinsey.
In 2019, a Denmark study of almost 7 million people found that women were diagnosed with hundreds of health conditions when they were on average four years older than men. The researchers believed that genetics, the environment, and gender bias could all be factors for the difference. Women spend 25% more of their lives in debilitating health versus men, according to a report from the World Economic Forum and the McKinsey Health Institute.
The gender gap research was backed up in May 2024 by a study published in The Lancet, which also found that women live longer than men, but spend more of their lives in poor health. The study quantified the health gap in terms of disability-adjusted life years (DALYs). It found that women were more likely than men to experience low back pain, depressive disorders and headache disorders, while men had higher DALY rates for mortality-driven conditions: road injuries, ischaemic heart disease, and COVID-19.
Closing the women’s health gap means increasing the diagnosis of women’s health conditions. Here are a few that have been under-diagnosed:
- Cardiovascular Disease and Heart Attack
Women are more likely to die after being admitted to hospital with a severe heart attack, and they are also less likely to be prescribed medications to prevent future heart attacks, such as statins. Research has found women were 50% more likely than men to be given an incorrect diagnosis following a heart attack.
- Endometriosis
Endometriosis affects 10% of women globally, but in the US, only 2 out of 10 cases are diagnosed. These diagnoses have taken more than seven years, and even longer for Black women. Many healthcare providers have told patients that their symptoms were in their heads or part of being a woman, or that the patient was exaggerating.
- ADHD
Attention deficit hyperactivity disorder (ADHD) has been misdiagnosed or under-diagnosed in females historically. ADHD symptoms present differently in women, while historically, research focused on boys with the condition and then applied to women. The ratio of males to females diagnosed with ADHD decreased nearly five-fold from 2010 to 2022, from males being 133% more likely to be diagnosed with ADHD than females in 2010 to 28% more likely to be diagnosed with ADHD in 2022.
- Autoimmune disorders
Autoimmune diseases are those that stimulate the body’s immune defences to attack itself and include lupus, psoriasis, multiple sclerosis, rheumatoid arthritis and thyroid diseases. They are the third most prevalent disease category after cancer and heart disease. Women account for 80% of people with autoimmune diseases, but it takes an average of five years for women to get a diagnosis, according to the American Autoimmune Association.
- Menopause and Women’s Health Issues
The level of underinvestment has been pronounced for health issues that predominantly or exclusively affect women.
Summary
Inequalities mean women are underdiagnosed, undertreated and underserved. More focus and investment are required to address the unique health needs of women, bridging the gaps in research, diagnosis, and treatment.



